Legionella and Legionnaire’s Disease

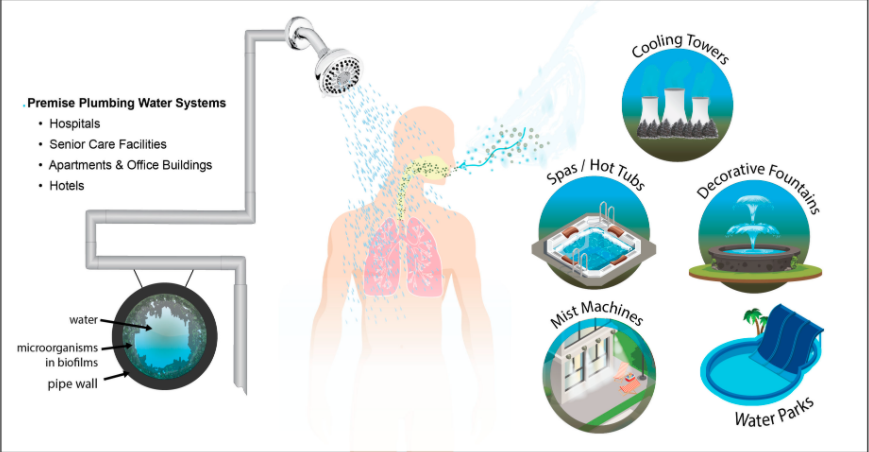
Legionella pneumophila is a gram-negative waterborne bacterium that causes Legionellosis, or Legionnaire’s Disease. Legionella species are found in nature, mostly in natural freshwaters (ponds, rivers…), and soils. But they are also found in artificial environments, where most cases of disease are linked to1. And here we are mostly talking about plumbing systems, like showers, toilets and sink faucets; which are the places where these bacteria grow and form biofilms, together with other organisms found in water systems, such as protozoa, algae and other bacteria1 (Fig.1).
Despite being showers the most common source of Legionella transmission indoors2, important Legionella outbreaks have happened through aerosol exposure from cooling towers, whirlpools, mist machines, and decorative fountains1 (Fig. 1). When inhaling aerosols containing the bacteria from hot or cold water systems, susceptible people can get Legionellosis, which can be manifested in two ways:
- Legionnaires’ disease (LD), which is a serious pneumonia with high mortality.
- Pontiac fever, which usually gives a mild flu-like illness without pneumonia, and usually does not need treatment.
There are more than 50 Legionella species currently, with more than 70 different serogroups3. Not all Legionella species cause disease. Nowadays, more than 20 species have been described as pathogenic, but the species Legionella pneumophila is the predominant one. It actually accounts for approximately 90% of confirmed cases of Legionellosis and, in particular, L. pneumophila serogroup 1 (sg 1)3
But, how prevalent this disease is? We can check some numbers in the last European Centre for Disease Prevention and Control (ECDC)’s report4. ECDC recollects data though annual retrospective data collection of Legionnaires’ disease cases in EU Member States, Iceland and Norway; and near real-time reporting of travel-associated cases of Legionnaires’ disease (TALD) through the European Legionnaires’ disease surveillance network (ELDSNet). Although Legionnaires’ is an uncommon and sporadic respiratory infection with an overall notification rate of 2.2 per 100 000 for the EU/EEA in 2018, the annual notification rate has increased from 2014 to 2018, from 1.3 per 100 000 in 2014 to 2.2 in 20184. The reports shows a 23% increase in the number of cases in 2018 compared with 2017, as well, with France, Germany, Italy and Spain being the countries that notified 71% of all cases in 20184 (Fig. 2).
For the U.S., the Centers for Disease Control and Prevention (CDC) have also reported a 4.5-fold increase in the number of Legionellosis cases from the period from 2000 to 2015 (0.42 per 100,000 persons in 2000 to 1.89 per 100,000 in 2015)5 (Fig.3).


According to the ECDC, the cause of this observed increase in EU/EEA, remains unknown. However, they hypothesize that it could be influenced by different factors, like the surveillance systems, an ageing population, increased travelling, climate changes affecting the ecology of Legionella and the design and maintenance in building infrastructures and water systems4.
Although Legionnaires’ disease is on the rise many businesses and individuals still ignore the risks associated with Legionella bacteria. Therefore, it is extremely important to conduct a risk assessment and test water systems for potential legionella. By doing so, we keep people/employees healthy, and follow the law!
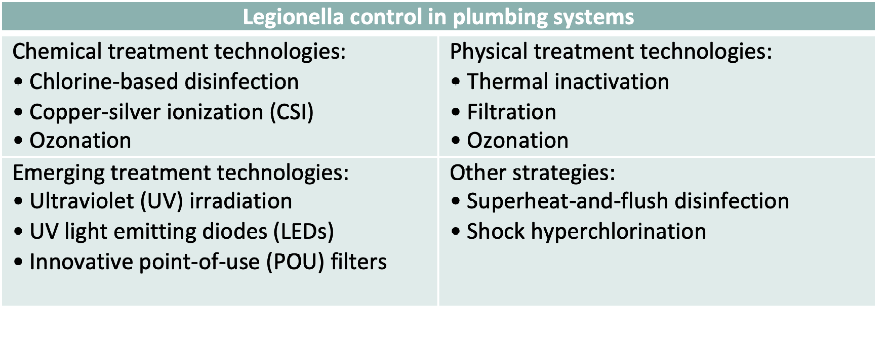
Monitoring potential pathogens in water systems is important and necessary, but we also need to treat the water in order to inactivate those. There are several technologies to control Legionella bacteria in plumbing systems, which are summarized in Table 1.
Chlorine has been widely used globally as a chemical disinfectant, serving as the principal barrier to microbial contaminants in drinking-water6. However, today we know that the combination of chlorine with organic compounds in drinking water produces chlorination disinfection by-products (DBPs)7 that can be harmful for our health8–15. Therefore, the levels of these compounds need to be monitored so they do not exceed a certain dangerous threshold. In addition to this possible health risk, there are several studies pointing towards the ineffectiveness of chlorine against Legionella1. To understand this, we need to go back into the heart of the problem: the pipe. As we saw in Fig.1, Legionella thrive in biofilms within the water pipes where it interacts with other bacteria and protozoa, like amoeba. Amoeba are microeukaryotes that prey on bacteria like Legionella. Some studies have shown that Legionella bacteria can survive inside amoeba, being protected from biocides such as chlorine16,17.
Therefore, in addition to risk assessment regulations it is important to consider alternative wate treatment products, so we can have safe and effective drinking water disinfection for the present future.
References:
- Carlson, K. M., Boczek, L. A., Chae, S. & Ryu, H. Legionellosis and Recent Advances in Technologies for Legionella Control in Premise Plumbing Systems: A Review. Water 12, 676 (2020).
- Hamilton, K. A. et al. Risk-Based Critical Concentrations of Legionella pneumophila for Indoor Residential Water Uses. Environ. Sci. Technol. 53, 4528–4541 (2019).
- Lee, H. K., Shim, J. I., Kim, H. E., Yu, J. Y. & Kang, Y. H. Distribution of Legionella species from environmental water sources of public facilities and genetic diversity of L. pneumophila serogroup 1 in South Korea. Appl. Environ. Microbiol. 76, 6547–54 (2010).
- ECDC. European Centre for Disease Prevention and Control. Legionnaires’ disease. In: ECDC. Annual Epidemiological report for 2018. (2020).
- Shah, P. et al. Legionnaire’s Disease Surveillance Summary Report, United States-Update July 2019. (2019).
- IPCS. Environmental Health Criteria 216 Disinfectants and Disinfectant by-products. (2000).
- Rook, J. J. Formation of haloforms during chlorination of natural waters. J. Water Treat. Exam. 23, 234–243 (1974).
- Morris, R. D., Audet, A. M., Angelillo, I. F., Chalmers, T. C. & Mosteller, F. Chlorination, chlorination by-products, and cancer: a meta-analysis. Am. J. Public Health 82, 955–63 (1992).
- Meier, J. R. Genotoxic activity of organic chemicals in drinking water. Mutat. Res. 196, 211–245 (1988).
- Bull, R. J. Health effects of drinking water disinfectants and disinfectant by-products. Environ. Sci. Technol. 16, 554A-559A (1982).
- Hildesheim Mariana E.; Cantor, Kenneth P.; Lynch, Charles F.; Dosemeci, Mustafa; Lubin, Jay; Alavanja, Michael; Craun, G. Drinking Water Source and Chlorination_Byproducts. Epidemiology 9, 29–35 (1998).
- Richardson, S., Plewa, M., Wagner, E., Schoeny, R. & Demarini, D. Occurrence, genotoxicity, and carcinogenicity of regulated and emerging disinfection by-products in drinking water: A review and roadmap for research. Mutat. Res. Mutat. Res. 636, 178–242 (2007).
- Cantor, K. P. et al. Polymorphisms in GSTT1, GSTZ1, and CYP2E1, Disinfection By-products, and Risk of Bladder Cancer in Spain. Environ. Health Perspect. 118, 1545–1550 (2010).
- Costet, N. et al. Water disinfection by-products and bladder cancer: is there a European specificity? A pooled and meta-analysis of European case-control studies. Occup. Environ. Med. 68, 379–385 (2011).
- Evlampidou, I. et al. Trihalomethanes in Drinking Water and Bladder Cancer Burden in the European Union. Environ. Health Perspect. 128, 17001 (2020).
- Shaheen, M., Scott, C. & Ashbolt, N. J. Long-term persistence of infectious Legionella with free-living amoebae in drinking water biofilms. Int. J. Hyg. Environ. Health 222, 678–686 (2019).
- Thomas, V. et al. Amoebae in domestic water systems: Resistance to disinfection treatments and implication in Legionella persistence. J. Appl. Microbiol. 97, 950–963 (2004).